[Image above] Credit: Partha S. Sahana; Flickr CC BY 2.0
No matter what your dental problem, science has you covered.
Need a filling?
Nanotechnology may soon swoop in to save your next cavity.
Researchers from the Universidade Estadual de Campinas in Brazil recently published a review of new research in nanodentistry, and the review highlights just how promising nanomaterials are in your mouth.
“Nanotechnology can be faced sometimes as a paradigm that promised a lot and delivered very little,” senior author Nelson Durán says in a press release from Cell Press. “The evolution of dental materials though nanotechnology is real and remarkable, reflecting on a billionaire market. In this way, dentistry was in fact one of the most benefited areas from the development of nanotechnology.”
For instance, nanocomposite resins containing silica and zirconia nanoparticles look more like the real dental deal and are less prone to fracture or loosening, according to the release. But there’s much more to come from nanodentistry and what it can do for our teeth, according to the review.
For instance, nanotech advances could help dental tissues repair themselves or could protect against infection. Nanoparticles incorporated into dental products could even help restore worn enamel or combat gum disease.
“Products could include antimicrobial adhesives made up of carbon nanotubes—creating a kind of wearable toothpaste—or quantum dots combined with cancer-specific antibodies that can be applied inside the mouth, emitting light if they detect any troublesome cells,” the release adds.
Safety and cost will be the remaining barriers to the new advances, but the authors contend that these hurdles can be overcome within the next few years.
That paper, published in Trends in Biotechnology, is “Advances in dental materials through nanotechnology: Facts, perspectives and toxicological aspects” (DOI: 10.1016/j.tibtech.2015.09.005).
In support of an increasing role of nanotechnology in dentistry, research from UCLA suggests that nanodiamonds could help maintain the strength and health of teeth after root canals.
During root canals, dentists drill into teeth in an effort to remove infected dental pulp inside the tooth. Afterwards, they fill the empty space with an inert polymer material called gutta percha—but the infected pulp isn’t always completely removed.
Persistent bacteria can continue to grow in small cavities within the pulp, leading to tooth loss and repeated dental procedures.
To help combat those problems, the UCLA researchers now report success in testing the ability of nanodiamond additives to reinforce conventional gutta percha. In addition, adding antibiotic amoxicillin to the nanodiamonds prevented bacterial growth in laboratory experiments.

A 3-D image of a tooth filled with nanodiamond-enhanced gutta percha, and an individual gutta percha point. Credit: Dong-Keun Lee; American Chemical Society
“The nanodiamond-enhanced gutta percha combines many desirable properties into a single platform, including vastly improved mechanical characteristics and the ability to combat bacterial infection following a root canal,” postdoctoral researcher Dong-Keun Lee says in a UCLA press release.
The team is currently optimizing the formula of their nanodiamond-loaded material and plans to begin clinical trials with the material in the next couple of years.
That paper, published in ACS Nano, is “Nanodiamond–gutta percha composite biomaterials for root canal therapy” (DOI: 10.1021/acsnano.5b05718).
Or perhaps a whole new tooth is in order?
3-D printing may be able to help.
Scientists at the University of Groningen in the Netherlands are working towards the ability to replace teeth with even more hygienic options—3-D printed teeth made of antimicrobial plastic.
To make sure the new custom teeth are safe, the scientists modified existing polymer dental resins by embedding them with quaternary ammonium salts, which have a positive charge that kills 99% of bacteria by disrupting their negatively-charged membranes, according to a New Scientist article about the research.
The paper detailing the work, published in Advanced Functional Materials, is “3D-printable antimicrobial composite resins” (DOI: 10.1002/adfm.201502384).
While composite materials are often cheaper than alternatives, they also don’t last as long—so ceramic materials are still an attractive alternative for faux teeth.
Researchers at ETH Zurich can now mimic the development of seashells, known for their incredible strength, to create synthetic ceramic teeth that more closely mimic their natural inspirations.
In particular, a component of seashells called nacre—or mother of pearl—is a popular biomaterial of interest. While nacre has been studied in depth (see here, here, and here), recreating the entire complexity and strength of a whole seashell is not so simple.
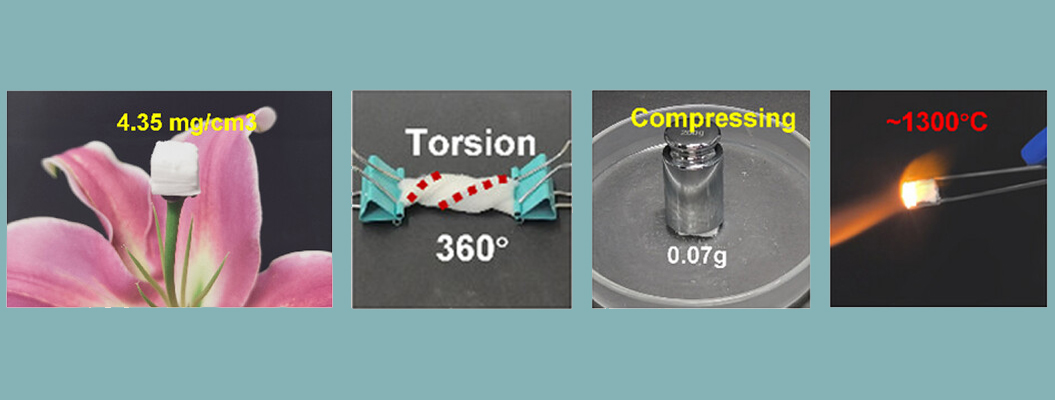
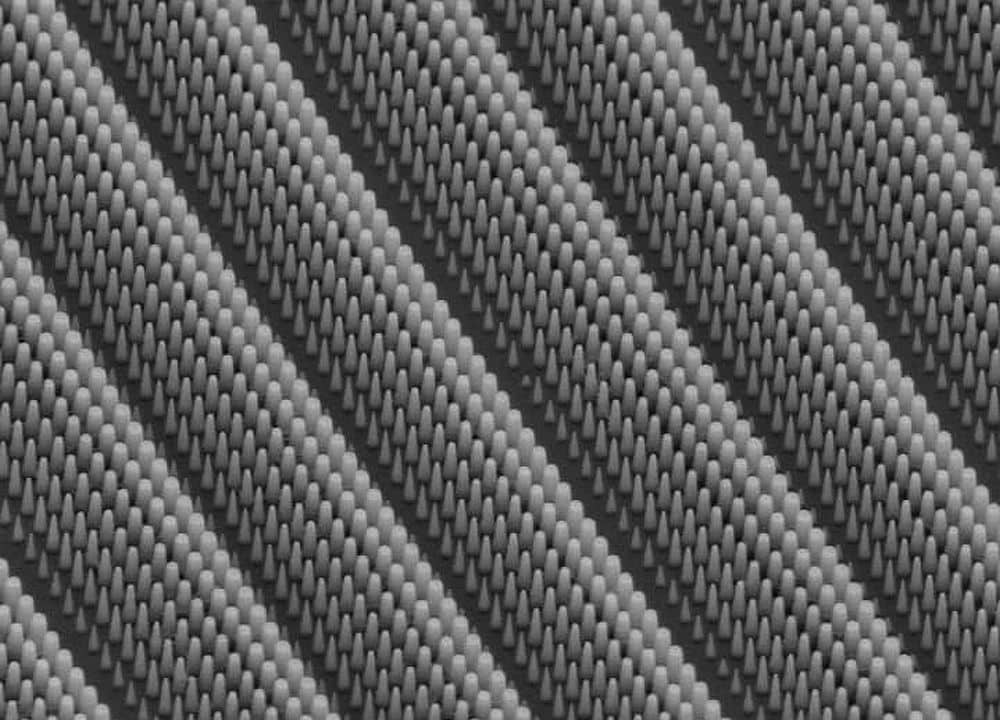
ETH scientists, however, have now recreated the complexity of multiple layers of organized ceramic microplatelets, seashell-style, with a new process they’ve called magnetically assisted slip casting (MASC).
In the technique, the team pours a suspension of magnetized ceramic platelets into a porous plaster mold. The porosity of the mold allows it to absorb liquid from the ceramic slurry, solidifying it from the outside in.
And now for the cool part—applying an alternating magnetic field to the liquid suspension during casting, before it solidifies, allowed the scientists to fabricate layers with alternating microplatelet orientations.

Electron micrograph of a crosssection of the artificial tooth. Ceramic platelets in the enamel are orientated vertically; in the dentin, they are aligned horizontally. Credit: Hortense Le Ferrand; ETH Zürich
The ability to create such a complex layered architecture inspired the team to then fabricate ceramic teeth that closely resemble the structure of natural teeth.
The team filled a plaster mold “with a suspension containing aluminum oxide platelets and glass nanoparticles as mortar,” according to an ETH press release. “Using a magnet, they aligned the platelets perpendicular to the surface of the object. Once the first layer was dry, the scientists poured a second suspension into the same mold. This suspension, however, did not contain glass particles. The aluminum oxide platelets in the second layer were aligned horizontally to the surface of the tooth using the magnet.”
Sintering the materials and filling remaining pores with a dental monomer completed the tooth. “The profile of hardness and toughness obtained from the artificial tooth corresponds exactly with that of a natural tooth,” says lead researcher André Studart in the release.

The natural tooth in its gypsum mold (left), the artificial tooth (sintered but not yet polymer infiltrated; middle), and a model tooth that has been sintered and polymer infiltrated (right). Credit: Tobias Niebel; ETH Zurich
The team is still working on improving the appearance of the material, but getting the microscopic organization correct is a considerable step forward.
The paper, published in Nature Materials, is “Magnetically assisted slip casting of bioinspired heterogeneous composites” (DOI: 10.1038/nmat4419).
Maybe a complete new set of chompers is needed?
No fear there, either.
Researchers from Georgia Institute of Technology and King’s College London are studying fish that develop teeth throughout their lifetimes with hopes of one day being able to activate tooth regeneration in humans, too.
The team is studying genes that control differentiation of teeth and taste buds, which arise from the same developmental tissue. The research with Lake Malawi chichlids shows that there is “developmental plasticity” teeth and taste buds.
The researchers are trying to better understand the pathways that control whether differentiation steers towards taste buds or teeth—with the hopes of one day being able to steer it.
“The exciting aspect of this research for understanding human tooth development and regeneration is being able to identify genes and genetic pathways that naturally direct continuous tooth and taste bud development in fish, and study these in mammals,” said coauthor Paul Sharpe in a Georgia Tech press release. “The more we understand the basic biology of natural processes, the more we can utilize this for developing the next generation of clinical therapeutics—in this case, how to generate biological replacement teeth.”
Author
April Gocha
CTT Categories
- Biomaterials & Medical
- Material Innovations
- Nanomaterials
Related Posts
Sports-quality ice: From pond side to precision Olympic engineering
February 12, 2026