[Image above] Credit: Bango Renders, StockSnap.io
Just like every other part of the human body, blood vessels experience wear and tear during normal operation. We are rarely aware of these minute changes, however, due to the body’s ability to initiate molecular activity that regenerates and repairs any damage.
Sometimes, though, the body fails to properly mend rips in the vessel wall. This failure to close the hole results in blood collecting in areas where it shouldn’t, leading to situations such as clots and aneurysms.
The sudden repercussions that can arise from this momentary bodily misstep hit home for me when my friend experienced an arterial dissection, which precipitated a stroke and required emergency hospitalization. Fortunately, after my friend took anticoagulant (blood-thinning) medication for several months, the body healed on its own without the need for stent insertion.
Throughout the entire diagnostic and treatment process, doctors relied on external imaging technologies to determine what was happening inside my friend. In vivo imaging is still an emerging modality for studying vascular structure and function, though intravascular ultrasound, which uses sound waves to capture real-time images from inside blood vessels, is becoming a more common diagnostic test.
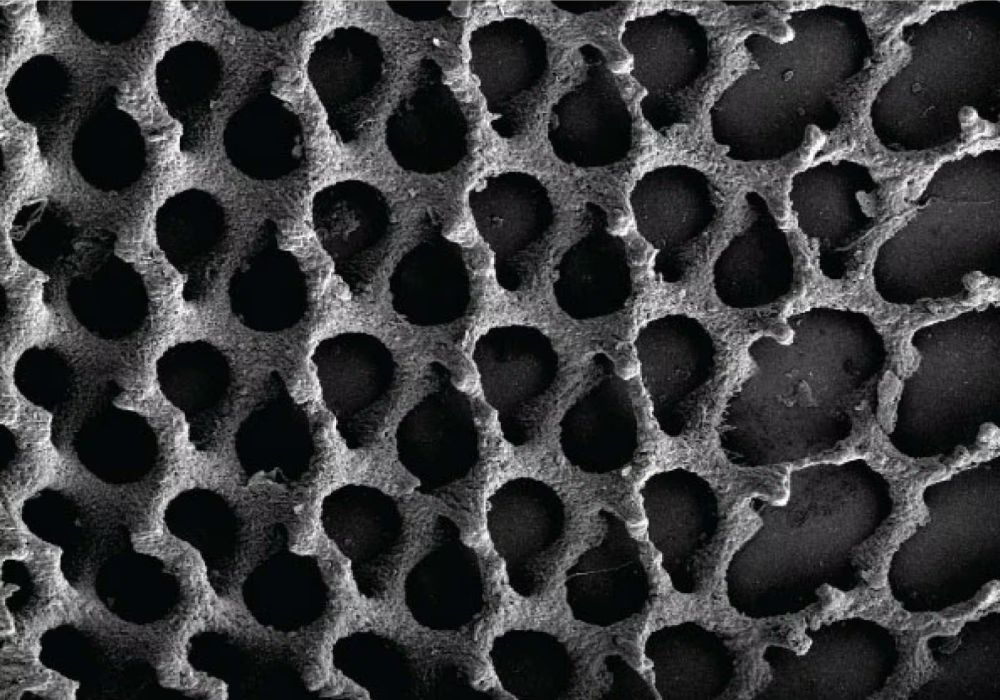
Optical coherence tomography (OCT) is another, newer intravascular imaging technique that uses near-infrared light to create images from inside blood vessels. A large-scale clinical trial in 2023 found OCT may be safer and lead to better outcomes for patients during stent insertion than the common angiography-guided procedure, which uses a special dye and X-rays to image blood vessels.
Despite these benefits, researchers struggle to adapt OCT for use inside the brain’s vasculature for several reasons. First, the fiber-optic probes used in OCT are typically quite stiff, making them too rigid to twist and bend through the brain’s convoluted passageways. Additionally, the torque cables, which rotate the OCT lens to image surrounding vessels and devices, are too large to fit inside the catheters that are telescopically advanced into the brain.
In a novel study published last week, researchers in the U.S. and Canada reported on the development and testing of a modified OCT approach that can be used inside the brain.
The new OCT method is the brainchild of Giovanni Ughi, assistant professor of radiology at the University of Massachusetts’ Chan Medical School in Worcester. He and his colleagues spent the past decade adapting OCT for use in the brain, which they did by altering the properties of the fiber-optic glass and devising a new system of rotational control that does away with torque cables.

This video shows the new OCT method being used to conduct an intracranial in-stent restenosis assessment. Credit: IEEE Spectrum, YouTube (from the supplementary materials of Pereira et al., Science Translational Medicine)
After initial testing in rabbits, dogs, pigs, and human cadavers, Ughi’s team sent the device to two clinical groups at St. Michael’s Hospital (Toronto, Canada) and Sagrada Familia Clinic (Buenos Aires, Argentina). Across the two groups, neurosurgeons treated 32 participants with various conditions arising from aberrant blood vessels by snaking the imaging probe through the patients’ groins or wrists and into their brains.
The new OCT procedure proved to be safe and well-tolerated across different anatomies, underlying disease conditions, and the complexity of prior interventions. In many cases, it provided information that led to actionable insights, such as achieving proper placement of stents that were not flush against the arterial wall.
“[This study] was a huge confirmation that the technology is ready to move forward,” says Ughi in an IEEE Spectrum article.
To advance this technology, Ughi is serving as senior director of advanced development and software engineering at startup Spryte Medical. The company is in discussions with regulatory authorities in Europe, Japan, and the United States to determine the steps necessary to bring the imaging probe to market.
The paper, published in Science Translational Medicine, is “Volumetric microscopy of cerebral arteries with a miniaturized optical coherence tomography imaging probe” (DOI: 10.1126/scitranslmed.adl4497).
Author
Lisa McDonald
CTT Categories
- Biomaterials & Medical