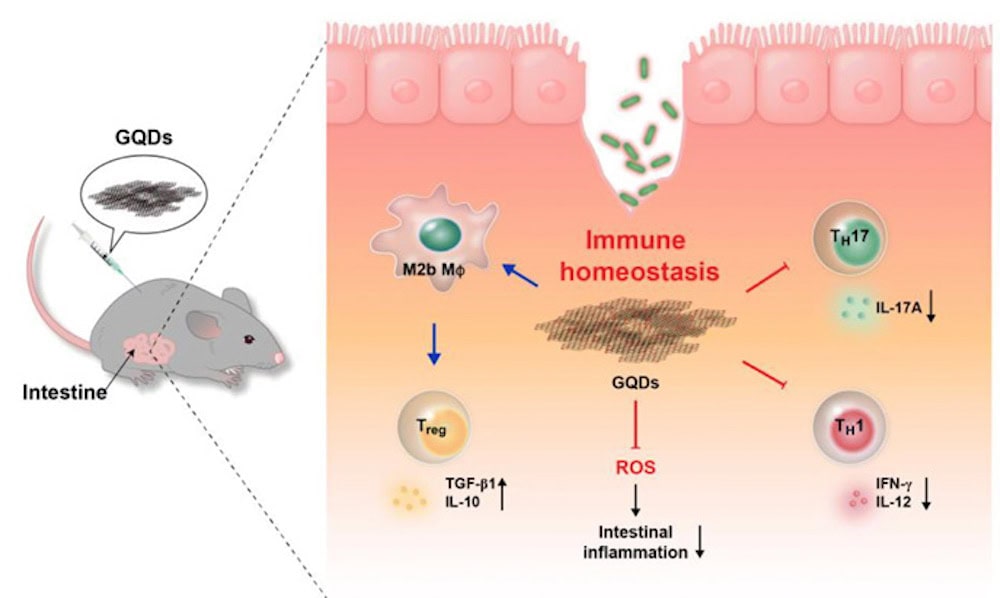
[Image above] Schematic diagram showing how graphene quantum dots (GQDs) affect a mouse colitis model, including preventing tissue degeneration and ameliorating intestinal inflammation. Credit: Lee et al., Science Advances (CC BY-NC 4.0)
As a science writer, I’ve followed news concerning the coronavirus SARS-CoV-2 and its accompanying disease closely. And I’m not only talking about the transmission mechanisms or bodily effects—I find the ways in which we socially handle the virus provides a deeper understanding of the situation and can help us realize more clearly the importance of scientific advances.
The response to COVID-19 in prisons and jails has particularly caught my interest. Correctional facilities account for some of the largest outbreaks in the United States, with one of the largest outbreaks happening in my adopted state of Ohio.
Compared to long-term care facilities, in which the risks to elderly residents are obvious, not everyone realizes that prisons and jails also consist largely of high-risk groups.
Since the 1990s, the percentage of inmates age 55 and older has increased drastically, from about 3% in 1999 to more than 10% by 2014. In addition, prisoners and jail inmates are more likely than the general population to report ever having a chronic condition or an infectious disease.
In the face of COVID-19, politicians and the public have given increased attention to these statistics, issuing calls to release vulnerable inmates that, unfortunately, have resulted in very few releases so far. But even during nonpandemic times, the ability of prisons and jails to care for their vulnerable populations is far from desirable.
One of the key factors preventing prisoners from receiving adequate healthcare is overcrowding. While the United States accounts for less than 5% of the world’s population, it has nearly 25% of the world’s prisoners. With so many prisoners, providing regular healthcare is difficult. But for prisoners with chronic conditions, which require ongoing medical attention, providing long-term individualized treatment is even less attainable.
Organizational and social reforms are necessary to reduce overcrowding and provide better healthcare to inmates. However, science also plays a significant role in solving the latter issue.
As mentioned above, prison and jail inmates are more likely than the general population to report ever having a chronic condition. And many chronic conditions, especially autoimmune diseases, still are not well understood. Thus, the more we learn about these conditions, the better treatments we can develop—ones that hopefully can be easily (and inexpensively) administered to inmates in prisons and jails.
To date, the exact cause of many autoimmune diseases is unknown. Instead, treatment focuses on controlling the immune system response. As such, much research on autoimmune diseases focuses on identifying and developing materials that provide control over the immune response.
In May, I wrote about research in Germany exploring effects of bioactive glass ionic dissolution on the immune system. In today’s CTT, I look at another material being investigated—graphene quantum dots.
Graphene quantum dots as anti-inflammatory therapy
Quantum dots are nanoscale particles made of a semiconducting material. Because of their size, quantum dots have different properties than larger particles due to quantum mechanics, which makes them a popular topic in nanotechnology research.
Traditionally, application development of quantum dots was hindered by high toxicity of the heavy metal ions used to create the dots. Fortunately, development of carbon quantum dots and graphene quantum dots has overcome this problem, as these dots have the advantages of nontoxicity, good solubility, stable photoluminescence, and better surface grafting.
Previous studies have shown the interaction of graphene quantum dots with immune cells, including macrophages and T cells. These results prompted the researchers of a new study to investigate graphene quantum dots as well.
The researchers, from Seoul National University in Korea, were interested in the ability of graphene quantum dots to treat inflammatory bowel disease (IBD), such as Crohn’s disease and ulcerative colitis.
They note in an open-access paper that immunosuppressive drugs are commonly used already to treat such diseases. However, “the treatments for IBDs are often accompanied by complications such as infections and malignancies,” they write.
“Thus, alternative drug with less side effects is still needed,” they add.
In their study, the researchers used the dextran sulfate sodium colitis animal model to investigate the inhibitory effects of graphene quantum dots on acute and chronic colitis. In this model, which is widely used in IBD research, dextran sodium sulfate is used to cause epithelial damage in mice, which induces a human ulcerative colitis-like response.
The researchers found that mice treated with graphene quantum dots experienced increased survival rates and reduced weight loss compared with untreated mice, and they scored lower on a disease activity index based on weight loss, activity, stool consistency, bleeding, and hair condition. In addition, the mice had lower levels of myeloperoxidase (a biomarker of ulcerative colitis) and reduced shortening of the colon—a characteristic feature of the disease.
In the paper, the researchers note several important factors that helped prevent tissue degeneration and intestinal inflammation in the graphene quantum dot-treated mice.
Suppressed excessive T cell activity
TH1 and TH17 cells secrete the proinflammatory cytokines IFN-γ and IL-17A, respectively, which both play a crucial role in intestinal inflammation.
The researchers found treatment with graphene quantum dots reduced proliferation of these T cells and secretion of proinflammatory cytokines.
Enhanced intestinal infiltration of regulatory T cells
Regulatory T cells protect tissues from inflammation and help promote tissue healing by suppressing activated proinflammatory immune cells.
The researchers found treatment with graphene quantum dots increased secretion of TGF-β1 and IL-10, which are major inducers and products of regulatory T cells and play a major role in alleviating colitis.
Switched macrophages from M1 to M2
M2-type macrophages, which have a role in recruiting regulatory T cells and their secreted cytokines, can help relieve the symptoms of colitis.
The researchers found treatment with graphene quantum dots suppressed the classically activated M1-like features of macrophages and converted them to anti-inflammatory M2 macrophages.

Experimental scheme for dextran sodium sulfate-induced chronic colitis and graphene quantum dot administration. Dextran sodium sulfate water (3.5%) was repetitively administered to mice to induce colitis. Graphene quantum dots were injected intraperitoneally (300 μg per head) 10 days after administration of dextran sodium sulfate. On day 27, mice were euthanized for further investigation. Credit: Lee et al., Science Advances (CC BY-NC 4.0)
In a Physics World article, the researchers say they are now looking to develop an oral version of the therapy and moving toward clinical trials.
“After studying the pre-clinical research this year, we are targeting stage 1 clinical trials in 2022,” Byung Hee Hong, professor and head of the Graphene Research Laboratory at Seoul National University, says in the article.
The open-access paper, published in Science Advances, is “Graphene quantum dots as anti-inflammatory therapy for colitis” (DOI: 10.1126/sciadv.aaz2630).
Author
Lisa McDonald
CTT Categories
- Biomaterials & Medical
- Nanomaterials