[Image above] Credit: Dirk Ribbler, Unsplash
As the coronavirus that causes COVID-19 continues to change and evolve, so too does our response to it.
Much research focuses on developing new vaccines to improve effectiveness and availability of COVID-19 protection. But changing how the vaccine is delivered is another way to improve protection as well.
For example, several groups of researchers in the United States, Canada, and China are investigating how to make COVID-19 vaccines inhalable. An inhalable vaccine has several perceived benefits to an injectable vaccine, including
- Halts infection at the body’s point of entry by inducing a localized immune response;
- Requires lower doses because of its localization, thus making it easier to produce;
- Makes mass vaccinations easier because it can be administered through disposable devices without the need for trained personnel; and
- Potentially, when stored in a dry powder form, could be kept stable for much longer than injectable liquid vaccines.
These benefits of inhalable COVID-19 vaccines extend to other inhalable medicines. And while some inhalable medicines such as epinephrine for treating mild symptoms of asthma are well established, researchers continue to investigate what other medicines could be modified for inhalable delivery as well.
In a new open-access paper, researchers from institutions in Italy, Greece, and Malaysia explored the development of inhalable drug-loaded calcium phosphate nanoparticles for treating myocardial cells in the heart.
Calcium phosphate is a family of minerals containing calcium ions together with inorganic phosphate anions, and sometimes hydroxide ions as well. It is the main mineral in human bone and teeth, and it is considered highly biocompatible.
The main medicinal application of calcium phosphate is for regenerating or replacing bone tissue. However, in 2018, some of the Italian authors of the recent study published an article demonstrating another use for calcium phosphate—as a drug carrier for treating the heart.
As explained in the earlier paper, scientists have made “remarkable advances” in the use of nanoparticles in the cancer field, but they have reported few preclinical tests for nanomedicine applied to treatment of cardiovascular diseases.
“The identification of innovative therapeutic nanoformulations, use of alternative administration routes, or a combination of both may help to overcome the limitations associated with current pharmacological treatments for [cardiovascular diseases] and lead to more specific and efficient therapies,” the Italian researchers write.
Peptide therapeutics is one treatment the researchers identified as facing limitations. Peptides are essentially smaller versions of proteins. They are of particular interest as therapeutic drugs because the body naturally produces many different peptides, thus therapeutic peptides are relatively well-tolerated and have fewer side-effects than other pharmaceutical compounds.
However, despite an increasing interest in peptide therapeutics, injection remains the main method for peptide delivery. The need for injection makes peptide therapeutics a less appealing option for diseases that require chronic, outpatient therapy.
In the 2018 paper, the researchers explored whether inhalation could be an effective method for delivering therapeutic peptides to the heart. They specifically looked at using calcium phosphate nanoparticles to carry the peptides because of the material’s biocompatibility, biodegradability, and ability to cross the cardiomyocyte cellular membrane, which they demonstrated in a 2016 paper.
The results of the 2018 study were promising—the peptide-loaded calcium phosphate nanoparticles successfully restored cardiac function in a mouse model. However, the researchers identified some limitations that needed to be addressed in future studies. Specifically, they acknowledged difficulties with controlling the size of peptide-loaded calcium phosphate nanoparticles before and after delivery.
In the new open-access paper, the researchers collaborated with colleagues in Greece and Malaysia to address the transient particle size challenge by turning the nanoparticles into a microparticulate dry powder through spray drying.
Spray drying is an extensively used solidification technique to produce microparticles containing nanoparticles with suitable properties as dry powders for inhalation. Spray dried particles demonstrate improved physical stability, have more predictable dose control, and allow the product to be used in home or care settings.
The researchers chose the diuretic mannitol as a soluble carrier for the calcium phosphate nanoparticles. They then explained the spray drying process and microparticle characteristics in detail.

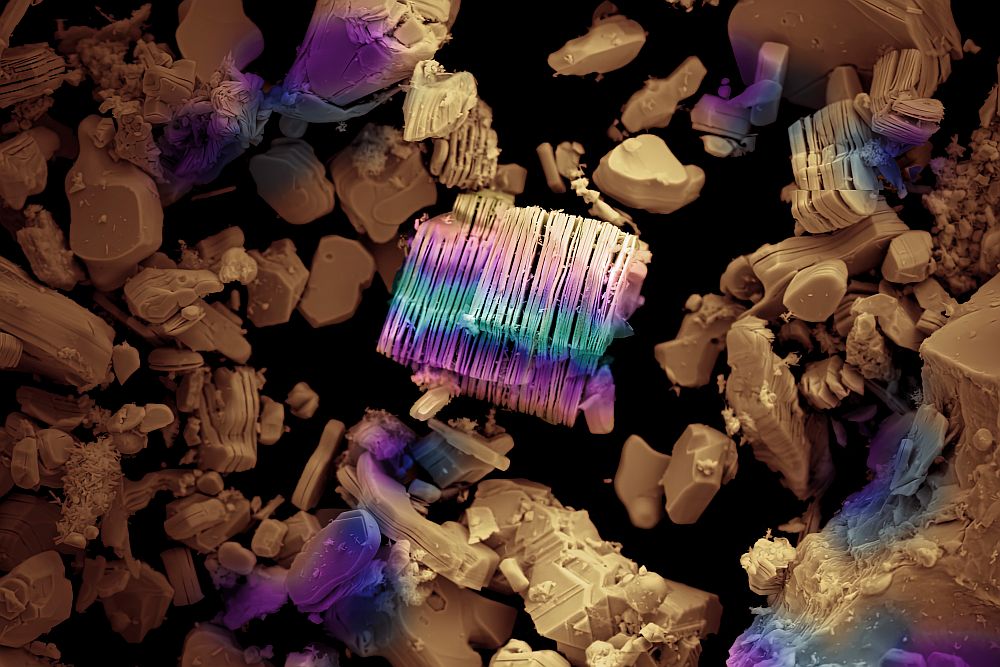
Scanning electron plan-view micrographs of doughnut-shaped microparticles with a calcium phosphate:mannitol ratio of 14:1. Credit: Quarta et al., Pharmaceutics (CC BY 4.0)
A key conclusion of the study was that mannitol protected the size of the released nanoparticles. In addition, increasing the mannitol concentration versus the calcium phosphate amount caused an increase in microparticle respirability, i.e., its ability to be breathed in.
“These quality attributes are crucial for the use of microparticles embedding nanoparticles for targeting the lung first and then the heart,” the researchers conclude.
The 2018 paper, published in Science Translational Medicine, is “Inhalation of peptide-loaded nanoparticles improves heart failure” (DOI: 10.1126/scitranslmed.aan6205).
The 2021 open-access paper, published in Pharmaceutics, is “Inhalable microparticles embedding calcium phosphate nanoparticles for heart targeting: The formulation experimental design” (DOI: 10.3390/pharmaceutics13111825).
Author
Lisa McDonald
CTT Categories
- Biomaterials & Medical
- Nanomaterials