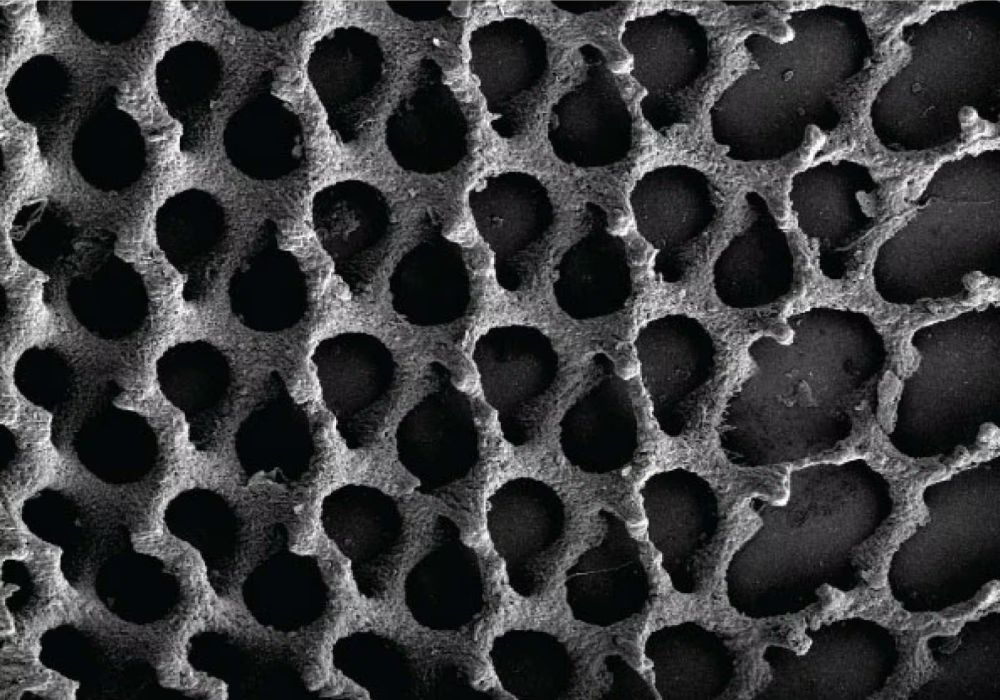
[Image above] A close up of 3D printed synthetic bone mimicking trabeculae, a major part of natural bone. Credit: Roohani et al., Advanced Materials (CC BY-NC 4.0)
Bone loss in humans is a widespread problem. Whether through disease, trauma, or just wear and tear over decades, an estimated 2.2 million orthopedic procedures involving bone grafting take place annually.
Autografts, or tissue taken from the patient’s own body, are generally preferred over synthetic grafts in many procedures due to their superior healing capabilities and lower risk of complications. However, in certain situations (described in more detail below), synthetic grafts are preferred.
To date, synthetic bone substitutes are mainly used for smaller and simpler grafting needs. The complex nanostructure of natural bone makes it both strong and elastic (to a point—ask the finger I once pinched in my garage door…). Achieving this combination of features with synthetic bone has so far been difficult, but a recent breakthrough by researchers at the University of Sydney in Australia sets a new milestone in the mission to create replacement bones.
From battlefield to biotech: A history of repair and rejection
The first recorded bone replacement procedure took place in 1668. A surgeon in the Netherlands, Job van Meekeren, used a piece of dog bone to repair a soldier’s damaged skull, and I was astounded to learn the Catholic Church later excommunicated the soldier for being part dog (only a few decades after Galileo’s trial for heresy).
Bone grafting procedures continued developing over the next 150 years. But it was during World War I and World War II that the field really took off as more soldiers became critically wounded and required advanced surgery.
Natural bone grafting has limitations. For one, harvesting the donor bone requires a second surgical site, doubling the risk of infection. And only so much donor bone can be taken from certain areas, limiting the extent of damage that can be treated this way. Additional bone can be sourced from another donor, but that introduces the possibility of rejection.
For these reasons, synthetic bone substitutes are preferred in some situations. But synthetic bones are not without their own challenges.
The challenge of mimicking nature’s masterpiece
The nanoscale structures in human bone tissue are the key to its mechanical strength and durability. Natural bone is made of an organic phase of collagen and an inorganic phase of hydroxyapatite nanocrystals. The two phases are intertwined, with the collagen providing structure and elasticity, while the hydroxyapatite nanocrystals provide strength.
Bone substitutes are produced in a variety of ways, ranging from electrospinning to 3D printing. Of the various bone substitute materials, calcium phosphates are widely used because of their biocompatibility and similarity to hydroxyapatite. However, they have low mechanical strength and generally are not great at encouraging osteoinduction, i.e., inducing stem cells to move in and create new bone tissue.
The reason that calcium phosphates typically fail to encourage osteoinduction is often attributed to their structure. As noted above, natural bone features complex nanoscale structures, which are difficult to achieve in synthetic bone substitutes. But studies on porous calcium phosphate grafts demonstrate the significant effect that micron- and submicron-scale pores can have on the material’s osteoinduction capabilities.
Current calcium phosphate fabrication methods cannot systematically and reproducibly incorporate these microstructural features into the material. As a result, “no quantified or robust consensus exists regarding the specific configuration of micropores or submicron-scale features that induces, if at all, osteoinduction,” the University of Sydney researchers write in their open-access paper.
Their new processing method overcomes this roadblock.
Bioceramic ink: A key to successful synthetic bone nanostructures
In the recent University of Sydney study, researchers led by Hala Zreiqat, professor of biomedical engineering and director of the ARC Training Center for Innovative BioEngineering, developed a 3D printing method to fabricate nanoarchitectured calcium phosphates.
They incorporated calcium phosphate bone prenucleation clusters with an average size of 5 nm into a printable, transparent resin at up to 80 wt.%. Then, two-photon polymerization was used to 3D print structures at 300 nanometers resolution, achieving unprecedented detail.
To minimize shrinkage during sintering, the researchers experimented with immersing the structures in simulated body fluid to induce apatite formation. The nanocrystalline apatite that forms in the simulated body fluid prefills the structural pores and increases the material volume prior to sintering, thereby acting as a densification aid.
Using this fabrication approach will allow systematic investigations of the mechanisms underlying osteoinduction in calcium phosphates, the researchers conclude in the paper. Ultimately, “Such advances could yield reproducible, osteoinductive CaPs [calcium phosphates] capable of reliably bridging critical-sized bone defects; an achievement that remains unattainable with current CaP ceramics,” they write.
In addition to enabling osteoinduction, reliable nanoscale fabrication of calcium phosphate is anticipated to increase its mechanical strength. This new technique therefore may also address the brittleness of calcium phosphate, allowing its use as a graft for larger sections of bone.
Toward a new era of bone regeneration
“The technology brings us a step closer to transforming bone graft surgeries in the future,” says Zreiqat in a press release.
I’m looking forward to seeing what future avenues of research this team pursues to continue advancing the field of bone grafts and regenerative medicine, leading to improved patient outcomes.
The open-access paper, published in Advanced Materials, is “Bioinspired nanoscale 3D printing of calcium phosphates using bone prenucleation clusters” (10.1002/adma.202413626).
Author
Becky Stewart
CTT Categories
- Biomaterials & Medical


