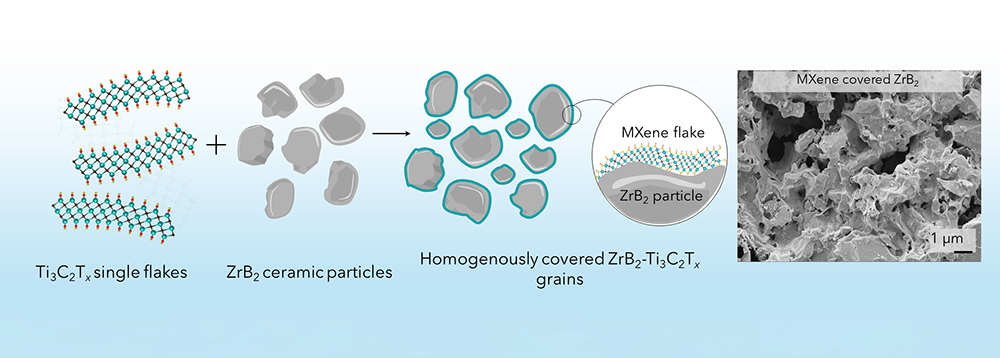
[Image above] Graphene oxide (orange) can effectively enter yeast cells and reduce the toxicity of harmful amyloid-β aggregates (light grey) by preventing amyloid-β accumulation and by increasing the cell’s ability to handle misfolded proteins and oxidative stress. Credit: Katharina Merl, Chalmers University of Technology
The human body is an incredible system, one that efficiently combines structural support, filtration capacity, energy generation, energy storage, electrical conductivity, gas exchange, processing power, dynamic flexibility, and regenerative potential into a single, adaptable unit.
Yet the materials that make up this system can sometimes fail due to overuse, injury, disease, or genetics—circumstances that are becoming more common as worldwide populations age.
When failure occurs, humans often turn to biomaterials to repair, replace, or enhance bodily materials. Ceramic and glass biomaterials serve many purposes in this regard, as detailed in the December 2020 Bulletin cover story, with ever more applications being identified.
One potential application for ceramic and glass materials is in the treatment of dementia, specifically Alzheimer’s disease.
Dementia is a general term for describing the progressive or persistent loss of intellectual functioning. Alzheimer’s disease, the most common cause of dementia, is a specific degenerative brain disease that is caused by complex brain changes following cell damage.
While researchers are still working to understand the full complexity of brain changes that occur in Alzheimer’s, one key part is the build-up of two substances inside the brain called amyloid-β (Aβ) and tau. When conditions in the brain are not right, these substances will clump up and form tiny structures called plaques and tangles, which make it harder for the brain to work properly.
Much Alzheimer’s research has focused on preventing the toxic aggregation of these substances (see overviews here and here). Recently, several Aβ-based therapies have received encouraging results. The U.S. Food and Drug Administration granted accelerated approval to the monoclonal antibody medication Aducanumab in June 2021, and in July 2023, the FDA granted traditional approval to the monoclonal antibody medication Leqembi.
Regarding ceramics, several in vitro studies demonstrated that graphene oxide (GO) has potential as an Aβ-based therapy. In these studies, GO sheets inhibited the Aβ fibrillization process through adsorption of amyloid monomers and by cutting mature amyloid fibrils.
An in vivo study using mice showed the potential of GO nanoflakes to ameliorate cognitive impairment through clearing the deposition of Aβ. But “the mechanism of this beneficial effect of GO nanoflakes has not been completely illuminated in vivo,” researchers write in a recent open-access paper.
The researchers come from Chalmers University of Technology in Sweden and the Technical University of Denmark. In their study, they investigated the impact of GO on intracellular Aβ aggregates and cytotoxicity using the yeast Saccharomyces cerevisiae as a model system.
Saccharomyces cerevisiae, colloquially know as brewer’s yeast or baker’s yeast, is useful for studying protein aggregation and proteostasis “[due] to a strong evolutionary conservation of the cellular protein quality control systems between yeast and humans,” the researchers explain.
They chose the Aβ42 form of Aβ to test their yeast model. Aβ comes in two major forms: Aβ42 and Aβ40, with 42 and 40 amino acid residues, respectively. With its two extra amino acids, Aβ42 is the more hydrophobic of the two and more prone to forming aggregates.
The researchers cultivated the Aβ42 yeast strain to early exponential phase and then mixed it with GO nanoflakes (average size of 90 nm). Scanning electron microscopy showed the cell surface was covered with GO flakes, but the cells retained their morphological integrity, indicating that the interaction with GO nanoflakes was not harmful. Transmission electron microscopy confirmed internalization of the GO nanoflakes by the Aβ42 cells.
Further analysis revealed that treatment with GO nanoflakes can diminish Aβ toxicity. The researchers propose that two independent pathways are behind this success, with the latter being driven by a presently unknown mechanism.
- Direct mitigation: the internalized GO suppresses Aβ42 aggregation.
- Indirect mitigation (mechanism presently unknown): the internalized GO boosts cellular machinery for coping with protein misfolding and oxidative stress.
To investigate the potential of GO to treat other causes of dementia, the researchers used another yeast model to explore GO’s ability to suppress HTT103QP aggregation, a hallmark of Huntington’s disease. Analysis of the model revealed that GO could help treat this disease as well.
“The findings offer insights for rationally designing GO nanoflakes-based therapies for attenuating cytotoxicity of Aβ42, and potentially of other misfolded proteins involved in neurodegenerative pathology,” the researchers conclude.
In a Chalmers press release, first author Xin Chen, researcher in the Division of Systems and Synthetic Biology at Chalmers, says the next step is to investigate whether they can develop a drug delivery system based on graphene oxide for Alzheimer’s disease.
“We also want to test whether graphene oxide has beneficial effects in additional models of neurodegenerative diseases, such as Parkinson’s disease,” she says.
The open-access paper, published in Advanced Functional Materials, is “Graphene oxide attenuates toxicity of amyloid-β aggregates in yeast by promoting disassembly and boosting cellular stress response” (DOI: 10.1002/adfm.202304053).
Author
Lisa McDonald
CTT Categories
- Biomaterials & Medical
- Material Innovations