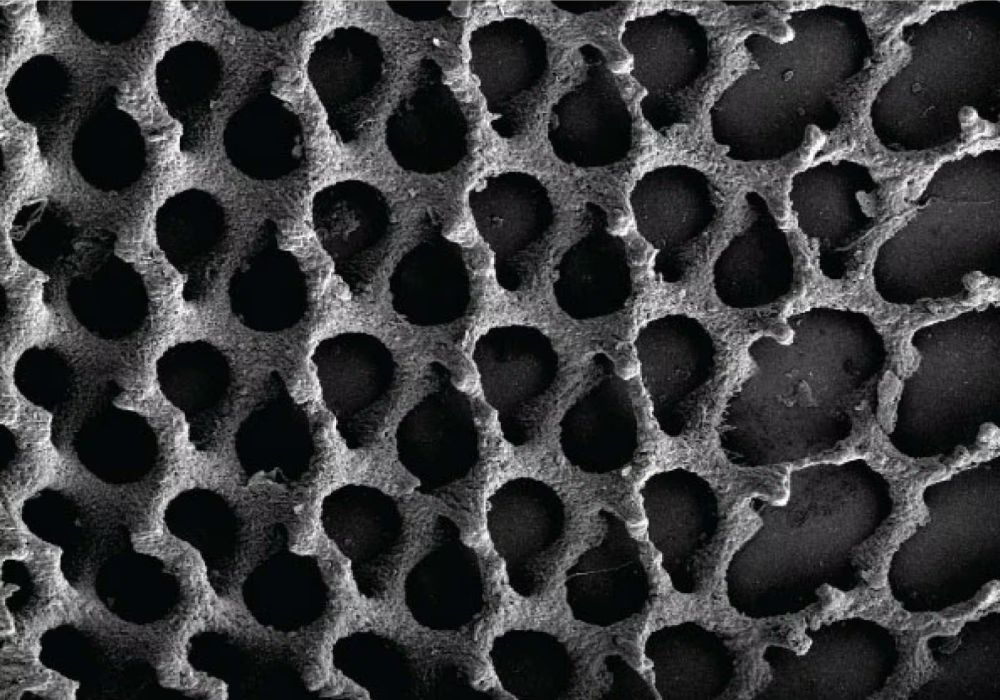
[Image above] Image of cells attached to a plate-like interfacial layer on bioactive glass. Researchers at Lehigh University began untangling the complicated interaction among structure, protein adsorption, and cell attachment in two papers. Credit: Thamma et al., Scientific Reports (CC BY 4.0)
When it comes to designing implants and scaffolds to aid in wound healing, the 3D architecture of the device plays an important role in tissue integration. Thus, it is no surprise that many studies focus on developing fabrication methods that allow for precise control over the device’s structure.
However, the relationship between device structure and biological performance is not always straightforward—particularly in the case of implants or scaffolds that contain bioactive glass.
When implants and scaffolds contain bioactive glass, a hydroxyapatite/carbonated hydroxyapatite (HA/CHA) interfacial layer forms on the device’s surface. Proteins from the blood and interstitial fluids quickly adsorb to the surface as well.
So, instead of the body’s cells interacting directly with the surface of the device, the interaction is mediated by this protein-filled interfacial layer. “These intertwined variables make the establishment of the role of nanostructure challenging and further complicate the design of optimum materials,” researchers write in a recent open-access paper.
The researchers come from Lehigh University and are led by Himanshu Jain, T.L. Diamond Distinguished Chair in Engineering and Applied Science and professor of materials science and engineering. He is joined by professor of cell biology Matthias Falk and doctoral students Tia Kowal (now postdoctoral researcher at Stanford Medicine) and Ukrit Thamma (now lecturer at King Mongkut’s University of Technology, Thailand).
In their study, they explain that they first began investigating the relationship among device structure, interfacial layer, and cell attachment in 2018, when they published a paper focused specifically on the first part of that relationship (device structure and interfacial layer).
In that paper, they fabricated nanoporous 30 mol% CaO–70 mol% SiO2 (30C70S) glass monoliths featuring the same specific surface area but different nanopore sizes (6–44 nm). Testing showed a complex influence of the nanopore size on formation of the interfacial layer.
“Due to pore‐size dependent diffusion of PO43− ions, two HA/CHA formation pathways were observed: plain deposition only on the surface, and formation of HA/CHA within the nanopores together with surface deposition,” they write in the 2018 paper. “The thickness of HA/CHA layer formed on the surface of a nanoporous glass monolith is determined by the pore‐size limited transport of Ca2+ ions that leach out via ion‐exchange from nanoporous glass substrates.”
In the new paper, they followed-up on these results by investigating the influence of the HA/CHA microstructures, “which form the interfacial layer between the cells and the underlying biomaterial,” on the attachment of MC3T3-E1 pre-osteoblast cells taken from mice. (Osteoblasts are cells that form new bone.)
They again used nanoporous 30C70S glass for the study, and they prepared them in such a way as to obtain HA/CHA layers with four different microstructures: long-needle, plate-like, flower-like, and short-needle. Testing revealed that the plate-like microstructure resulted in the highest average density and size of attached pre-osteoblast cells by a noticeable amount, followed by long-needle, short-needle, and flower-like, respectively.
These results would appear to suggest a straightforward correlation between HA/CHA microstructure and cell attachment. However, the researchers point out that the plate-like and flower-like microstructures, which demonstrated significantly different cell attachment percentages, are similarly shaped. Thus, “cell attachment and adhesion do not simply correlate with HA/CHA morphology.”
Additionally, the researchers point out that in real-world application, proteins spontaneously adsorb onto the biomaterial surface long before cell attachment, proliferation, or differentiation occurs. “Therefore, in order to explain the differences in cell attachment and adhesion on different HA/CHA microstructures, it is advantageous to understand how the amount and structure/conformation of adsorbed proteins is affected by HA/CHA microstructures,” the researchers write.
When the researchers tested the adsorption of three different types of proteins to the HA/CHA microstructure, they found that the long-needle microstructure had the highest adsorption percentage, with plate-like coming in third place behind short-needle. When the previously acquired cell attachment data was plotted as a function of the average percent adsorption of proteins, the trendline fit poorly, “indicating that cell attachment does not correlate closely with the amount of adsorbed [proteins].”
Because amount of adsorbed protein could not account for cell attachment, the researchers then looked closely at the shapes of the adsorbed proteins using attenuated total reflection Fourier transform infrared spectroscopy. This line of inquiry led to a breakthrough.
The researchers found there was a positive correlation between the level of cell attachment and the fraction of the protein bovine serum albumin (BSA) in its β-sheet structure. “Though BSA is not believed to play a direct role in facilitating cell attachment, … As the β-sheet/α-helix ratio increases, the density and average size of attached cells increase, suggesting that the unfolding of BSA upon adsorption enhances initial cell attachment,” the researchers write.
How the HA/CHA microstructures influence the shape of the adsorbed proteins is not fully clear at this point, but a possible explanation is that variations in the interfacial layer’s Ca2+/PO43− ratios can attract different functional BSA polypeptide groups, “leading to different conformations of BSA absorbed on various HA/CHA microstructures.”
In sum, the researchers report that “cell response, as quantified by cell attachment and morphology, does not correlate with nanopore size, nor HA/CHA layer micro/nano morphology, or absorbed protein amount (bovine serum albumin, BSA), but with BSA’s secondary conformation as indicated by its β-sheet/α-helix ratio.”
In a Lehigh press release, Jain explains why the results are so significant.
“There are others who have studied the interfacial protein layer,” he says, “but this work showed directly and unambiguously for the first time how some specific nanoscale features of the substrate can impact the secondary molecular structure of the proteinated interface that in turn affects the response of the cells that are thousands of times larger.”
The 2018 paper, published in Journal of Biomedical Materials Research, is “Influence of nanoporosity on the nature of hydroxyapatite formed on bioactive calcium silicate model glass” (DOI: 10.1002/jbm.b.34184).
The 2021 open-access paper, published in Scientific Reports, is “Nanostructure of bioactive glass affects bone cell attachment via protein restructuring upon adsorption” (DOI: 10.1038/s41598-021-85050-7).
Author
Lisa McDonald
CTT Categories
- Biomaterials & Medical