[Image above] There are more than 50 nanomedicine products currently approved for clinical use, including mRNA vaccines to immunize against coronavirus, which were made possible by lipid nanoparticles. Credit: Mufid Majnun, Pexels
The ethics of nanotechnology is a topic we’ve touched on frequently this year, starting with the April 2024 issue of Ceramic & Glass Manufacturing. Its ability to improve the functionality and performance of devices is starting to materialize in many industrial sectors, but commercial scale-up is also shining a light on the potential health risks of working with these materials.
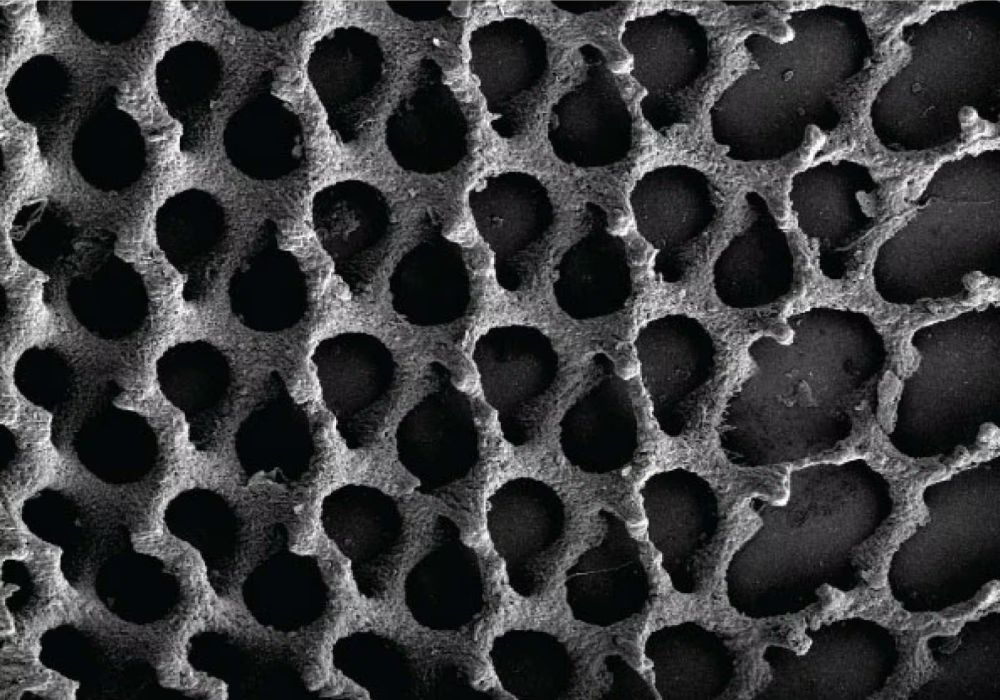
Researchers and policymakers alike are especially sensitive to the risks of nanotechnology in the medical field. Even though nanomaterials may help treat illnesses and diseases that we’ve long struggled to cure, such as dementia, there can be unexpected side effects from working with the nanoforms of traditional bulk materials, such as titanium dioxide. Transitioning nanomedicine into clinical use, then, requires a better understanding of the material’s physicochemical properties and behavior when exposed to different cells or tissues.
Fortunately, we are now at a stage where the (un)successful translation of nanomedicines into practice has generated a ton of knowledge on overcoming the common hurdles encountered during nanomedicine development. By compiling this knowledge, a global team of expert scientists in academia and industry recently developed a set of standards to help slash costs and reduce the time it takes to develop nanomedicine treatments and make them available for patients.
The so-called DELIVER framework, as described in a recent paper, comprises core principles for early-stage development. By following these guidelines, researchers will be able to more quickly “deliver nanomedicines to clinical development, regulatory approval, and market registration,” the authors write.
The principles are categorized as either “Essential,” “Important,” or “Useful.” For example, while it is “Essential” to use biocompatible and nontoxic nanomaterials, using biodegradable nanomaterials is only considered “Important,” while a “Useful” practice is undertaking silico toxicity screening.
The authors note that the DELIVER framework’s emphasis on early-stage development complements existing guidelines for late-stage development, such as those by the U.S. Food and Drug Administration and the International Organization for Standardization. However, they emphasize that the framework should not be used to advocate against exploratory or “blue sky” research activities that have no or little intention of immediate clinical translation.
“Fundamental research is critical for progressing the field of nanomedicine and is necessary to uncover the underlying mechanisms that underpin nanomedicine efficacy and toxicity, as well as contribute to radically new concepts and solutions,” they write. “Fundamental investigators must continue to develop and explore novel nanomedicines and inform translational investigators of the mechanisms driving disease pathology, the bio-barriers limiting therapeutic efficacy, the need for patient stratification, and the future strategies that can be employed for optimizing nanomedicines efficacy.”
The paper, published in Nature Nanotechnology, is “A translational framework to DELIVER nanomedicines to the clinic” (DOI: 10.1038/s41565-024-01754-7).
Author
Lisa McDonald
CTT Categories
- Biomaterials & Medical