[Image above] Credit: Scot Casey; Flickr
When it comes to repairing the human body, how the body interacts with a material is just as important—if not more important—as the material itself.
That theme was prominent throughout the variety of excellent technical talks at last week’s Innovations in Biomedical Materials meeting in Chicago, Ill. So it’s no surprise that the theme also rings true throughout the larger biomedical materials research community.
Repairing large-scale bone defects is one area of biomedical materials research that is still searching for just the right material. Doctors have decently sufficient tools to repair smaller bone defects, but large voids are a major challenge.
For large bone defects, it’s almost as if the body doesn’t know where to start—it has trouble laying down new bone, because there’s nothing to build upon.
So researchers have tried to give the body a helping hand by developing porous scaffolds that can fill large voids, allowing the body’s own cells to infiltrate and repair the bone.
Researchers have explored various scaffold materials for their suitability as a bone stand-in, including hydroxyapatite. And earlier this year, we saw that bioglass may even be promising for large-scale bone defects.
Now researchers at Drexel University (Philadelphia, Pa.), along with collaborators at the University of Sydney in Australia, are looking to the body’s immune system for insight into why some of these scaffold materials work better than others.
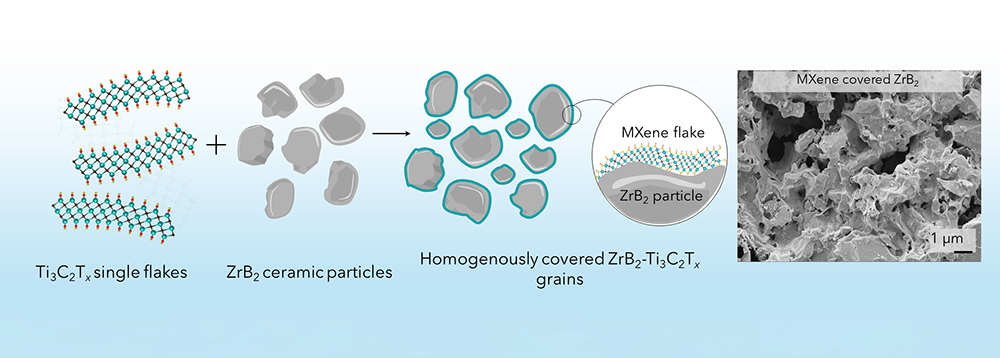
The team is exploring new scaffold materials that they now show can better stimulate bone to repair itself. According to a Drexel University press release, the researchers are experimenting with baghdadite (Ca3ZrSi2O9) and strontium–hardystonite–gahnite (Sr–Ca2ZnSi2O7–ZnAl2O4) ceramic scaffolds, which University of Sydney researchers developed and have previously shown can promote bone regeneration in animals.
“We wanted to know why these scaffolds were successful and to understand the contributions of macrophages to that process,” Kara Spiller, associate professor of biomedical engineering at Drexel and senior author of the new study, says in the Drexel release. “Once you understand those mechanisms, you can apply the information to regenerate other types of tissue besides bone.”
Macrophages are the immune system’s cleanup crew—they’re a type of white blood cell that gobbles up junk within the body, such as bacteria, cellular debris, and foreign particles. They’re a really important component of the body’s immune system because they neutralize stuff and help the body get rid of it.

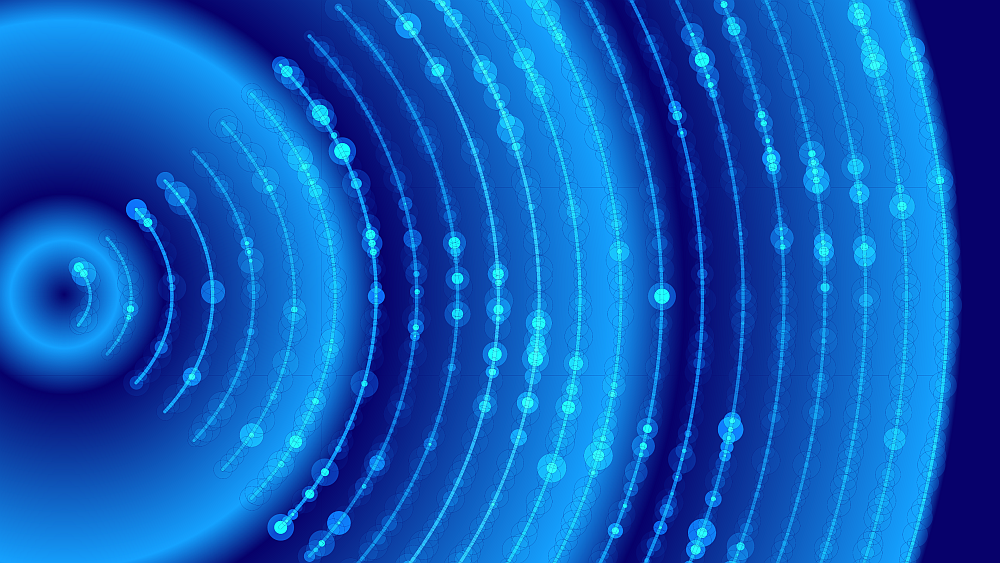
Confocal microscope image of macrophages engulfing fluorescent beads. Credit: ZEISS Microscopy; Flickr CC BY-NC-ND 2.0
The scientists examined how the new scaffold materials compared to tricalcium phosphate–hydroxyapatite (TCP-HA) bone scaffolds, which are used clinically. By growing human macrophages on the three kinds of scaffolds in the lab, the team could measure how each material affected macrophages’ gene expression.
In comparison to TCP-HA scaffolds, the new baghdadite and strontium–hardystonite–gahnite scaffolds activated the cells to transform into a particular variety called an M2c macrophage.
Macrophage transactions—like much of the human immune system—are a complex sequence of events. But the important point here is that M2c macrophages are known to have a hand in tissue repair and remodeling. So the presence of M2c macrophages on the bone scaffolds indicates that these materials are better suited to catalyze repair.
Watch the brief animation below to see how well the macrophages (aqua-cored dots) attached to one of the bone scaffolds after just six days.

Credit: Drexel University; YouTube
Further experiments showed that direct contact with the scaffold materials themselves, rather than soluble factors released by the materials, causes the macrophages’ transformation.
“The macrophages degrade the scaffolds and shape them into something new,” Spiller says in the release. “And that’s the holy grail of tissue engineering—that you make a scaffold that replaces itself with healthy tissue.”
The results suggest that certain materials can better stimulate the body to repair itself, so choosing the right scaffold material is of utmost importance to optimize healing and tissue repair.
But what is it about the new scaffolds that promote immune cells that are favorable for healing?
That’s to be determined—according the release, the researchers will next probe whether the composition, texture, or other features of the scaffolds are responsible for macrophage activation.
The paper, published in the Journal of the Royal Society Interface, is “In vitro response of macrophages to ceramic scaffolds used for bone regeneration” (DOI: 10.1098/rsif.2016.0346).
Author
April Gocha
CTT Categories
- Biomaterials & Medical
- Material Innovations